Abstract
Background: Primary central nervous system lymphoma (PCNSL) is a rare and aggressive subtype of B-cell lymphoma with very poor survival. Genetic alterations often occur in the chronic active B-cell receptor signaling which mediate the response to BTK inhibition (BTKi) in PCNSL. However, the efficacy of high-dose methotrexate as a first-line treatment was suboptimal with a short effective remission time and low response rate. We aimed to investigate the efficacy of induction treatment, high-dose methotrexate in combination with ibrutinib and temozolomide (MIT), in newly diagnosed PCNSL.
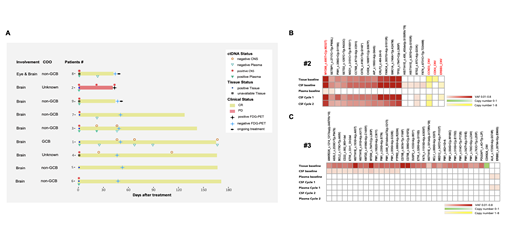
Methods: Thirty-three patients were planned to be enrolled in this open-label, non-randomized, multi-center phase II prospective clinical study (NCT04514393). Between October 2020 and April 2021, nine newly diagnosed PCNSL patients were enrolled. Eligible patients are ≥18 and ≤75 years of age with adequate organ function and require at least one measurable lesion. The MIT induction treatment included six cycles of high-dose methotrexate (HD-MTX, 3.5 g/m 2, every three weeks), ibrutinib (560 mg/d, after HD-MTX clearance), and temozolomide (150 mg/m 2 d1-d5, every three weeks). After the completion of the six cycles of MIT induction treatment, ASCT consolidation (only for patients < 65 yr) and daily ibrutinib (560 mg/d) were administered up to two years, or until disease progression, intolerable toxicity, or death. Treatment response was evaluated by brain MRI and FDG-PET and/or cerebrospinal fluid (CSF) examination every two cycles of the induction MIT treatment. The primary objective of this study was to evaluate the overall response rate (ORR) of MIT induction treatment for PCNSL defined as the proportion of subjects with complete response (CR) or partial response (PR). The safety and toxicity of MIT treatment were also investigated. No dose reduction or delayed treatment occurred. Baseline tissue samples and sequential CSF/plasma samples were collected and underwent targeted next-generation sequencing (NGS).
Results: The median age of the nine enrolled patients was 50 yr (range: 29-68) and six of them were male. Six patients have completed the six cycles of MIT treatment and the rest three had just completed two cycles. Hematologic toxicity was mild, Grade 3-4 neutropenia occurred in one patient. Other side effects such as opportunistic infections (including Aspergillus) were not observed. Eight out of the nine (88.9%) patients achieved CR. While patient #2 progressed and dropped out after two cycles of MIT treatment (Figure A). The mutational profiles of baseline tissue and/or CSF samples revealed that PIM1 and MYD88 mutations were present in 88.9% of the entire cohort followed by HISTHIE and CD78B (6/9, 66.7%). CDKN2A copy number loss was detected in four patients. Four patients with sequential CSF or plasma sampling during MIT treatment were analyzed for dynamic disease monitoring. As shown in the figure A, the clearance of ctDNA in the CSF/plasma samples was observed as early as post one cycle in three CR patients (#1,3,4) and maintained until the latest follow-up. However, the ctDNA remained detectable in the CSF sample of the PD patient (#2), which baseline genetic status shows MYD88 (M232T) mutation alone without CD79B mutations, and with CCND3, CDK4 and ERBB3 gene amplification(Figure B). After a median follow-up of 7 months, the 1-year PFS is 88.9% and the OS is 100%. Other clinical results of this ongoing study (NCT04514393) will be updated.
Conclusions: The induction treatment of MIT achieved excellent responses in newly diagnosed PCNSL patients with mild hematologic toxicity. The clearance of ctDNA in CSF/plasma samples was observed during dynamic disease monitoring which was in accord with imageology-based response evaluation.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal